A recent report from the U.S. Department of Justice revealed alarming rates of mental health disorders among jail inmates–on average, 44 percent of inmates had a mental health diagnosis. Despite this prevalence, jails lack adequate resources to meet inmates’ mental health needs, potentially worsened by discriminatory practices, implicit bias, overcrowding, and hostile environments. And these challenges disproportionately affect racial and ethnic minorities. Further, jails are major public safety expenditures. Michigan, for example, spent an average of $35,809 per inmate in 2015.
In the piece, CHRT outlines three justice reform approaches adopted by the Washtenaw County Sheriff’s Office, with funding from the county’s Public Safety and Mental Health Preservation Millage, that have emerged as promising solutions to reduce overcrowded jails, address systemic bias, reduce recidivism, and save taxpayer dollars:
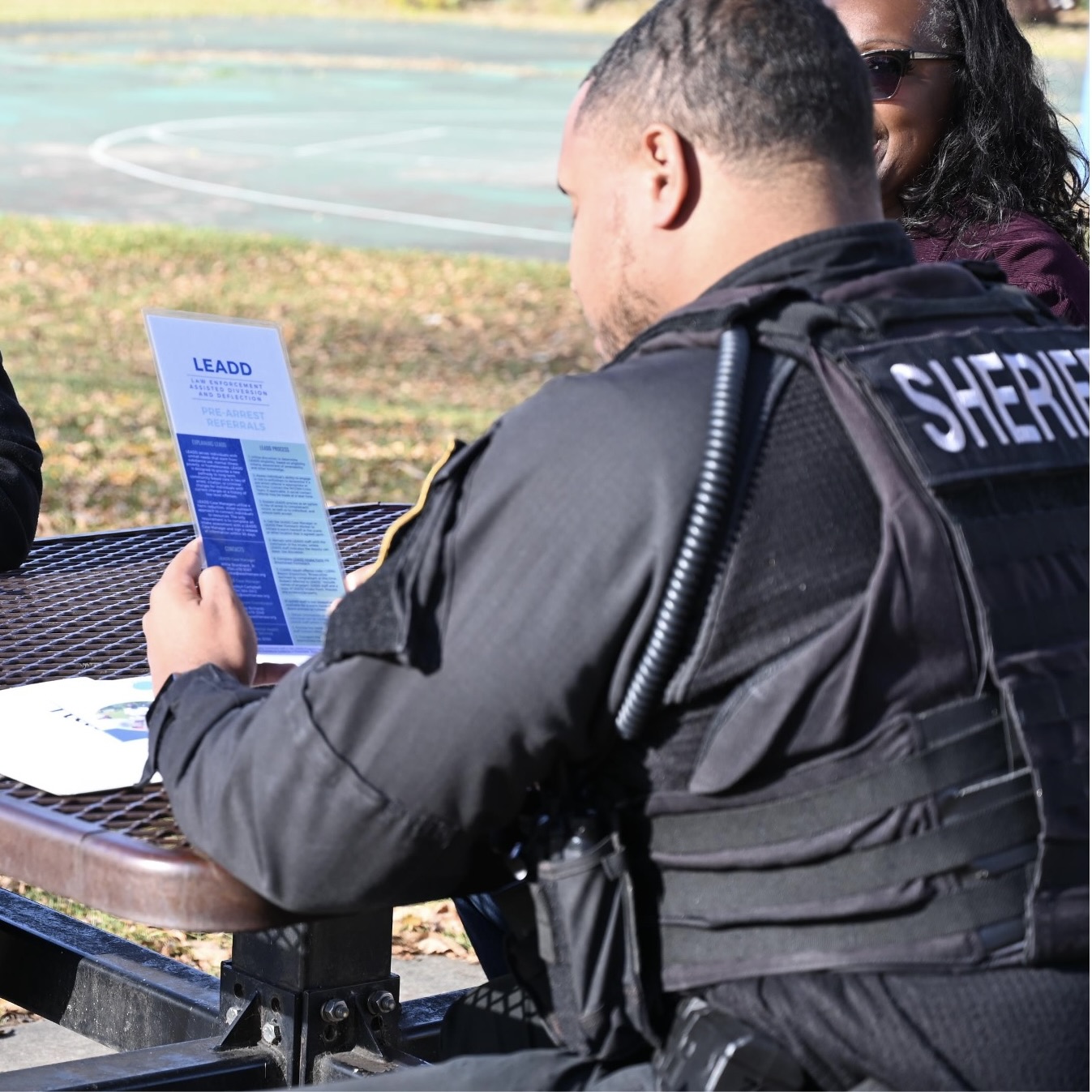
- Diversion programs, which divert those with criminal justice involvement into community supports,
- Deflection programs, which deflect those at risk of criminal justice involvement into community supports, and
- Reentry programs, which get individuals in jail the help they need to successfully return to the community.

 In the U.S., there are not enough behavioral health workers to meet the demand for mental health and substance use services, particularly in rural areas.
In the U.S., there are not enough behavioral health workers to meet the demand for mental health and substance use services, particularly in rural areas.
 The Michigan government has jurisdiction over a wide array of health policy issues. From the regulation of insurance products, to oversight of the state’s Medicaid program, to investing in local public health efforts, Michigan policymakers craft policies and budgets that impact the health of millions of Michiganders.
The Michigan government has jurisdiction over a wide array of health policy issues. From the regulation of insurance products, to oversight of the state’s Medicaid program, to investing in local public health efforts, Michigan policymakers craft policies and budgets that impact the health of millions of Michiganders.
 The Bipartisan Budget Act was signed into law on February 9, 2018. While the main purpose of the legislation is to temporarily fund the federal government through March 23, 2018, it also includes an agreement to raise the caps on domestic and military spending for the next two years.
The Bipartisan Budget Act was signed into law on February 9, 2018. While the main purpose of the legislation is to temporarily fund the federal government through March 23, 2018, it also includes an agreement to raise the caps on domestic and military spending for the next two years.
 One in five Michigan residents report having been diagnosed with depression at some point in their lives. Mental health disorders cause more disability among Americans than any other illness group.
One in five Michigan residents report having been diagnosed with depression at some point in their lives. Mental health disorders cause more disability among Americans than any other illness group.